San Diego Heart and Vascular Associates
An Association of Independent Physicians
Hospital Therapies

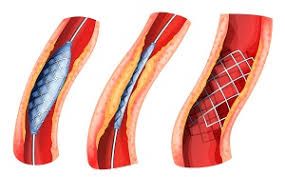
Cardiac Catheterization / Stents
What should you expect?
The doctor will insert a tiny, flexible plastic tube called a catheter through an artery in the groin, leg, or arm. A special dye is injected so blood flow through the arteries is visible on the TV monitors. The doctor moves a balloon catheter, and then a stent, to the site of the blockage. The balloon is inflated and stretched wide against the artery walls, which opens the blockage. Then the balloon is deflated and taken out, leaving the stent in place.
During the procedure, the doctor will insert the balloon catheter and inflate it to open the blockage. A stent will then be guided to the site. The doctor may need to use a number of stents to open the whole blocked area. You may feel some discomfort when the balloon is inflated. This will go away when the balloon is deflated. A small tube called a sheath may stay in the artery for two to four hours after the procedure. In some patients, it will stay in place overnight.
After the procedure, you may go to the recovery area or to your hospital room. You must lay flat on your back while the sheath is in place. The head of the bed may be tilted up a little to help you rest. You will be able to bend the other leg to relieve pressure on your back, or the nurse may roll you on your side. When it is safe to remove the sheath, the doctor or nurse will apply pressure to the area for 20 to 30 minutes. A dressing may then be applied.
Peripheral Angioplasty
This procedure involves a balloon angioplasty; however, this procedure is performed on a vessel outside of the heart, for example the leg vessels.
This procedure widens or opens narrowed blocked arteries. Your doctor may suggest this procedure if you have peripheral artery disease (PAD), which can cause:
- Chronic pain in your legs.
- Heavy feeling in your legs.
- Limitations to your daily activities.
- Wounds on your legs or feet that do not heal.
Balloon Angioplasty
What should you expect?
Make sure your doctor is aware of all medications you are currently taking—both prescription and over the counter. If your doctor instructs you to take any medications, take them with a small amount of water. If you have allergies, make sure your doctor is aware—especially drug allergies.
Make arrangements for a friend or family member to drive you home.
You may receive medication through an IV to relax you. A small incision is made in the groin area, into which a catheter is inserted. A catheter is a thin tube that the doctor will slide through an artery. A dye is injected so that an angiography(X-rays) can be taken.
A small balloon is inserted through the catheter to the area of blockage. The balloon is inflated and deflated, while pressure is applied to the insertion site. This compresses the plaque which causes the blockage..
After your angioplasty, in the recovery area, pressure is applied to the area of blockage for approx. 15 minutes. You will need to lie still, keeping your leg straight for a few hours. You may go home the same day, or spend the night in the facility.
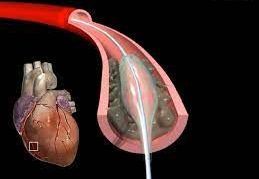
Transcatheter Aortic Valve Replacement (TAVR)
There are several ways your doctor can perform TAVR, depending on your health and the health of your blood vessels.
A TAVR using the femoral artery, a blood vessel in your groin or thigh, is the most common. Your doctor guides a tube with the replacement valve through the femoral artery to the heart.
Blood vessels in the chest may be used by the doctor to guide the tube to your heart, if your femoral artery is too small or damaged. This approach is called transapical access.
Stomach area blood vessels may be used for TAVR if a patient’s leg arteries are too small or diseased for a more standard approach. NHLBI researchers developed this approach, called transcaval access, to make TAVR available to high-risk patients. It is less common. The doctor makes holes in both the vena cava, a major veins in your stomach area, and the nearby aorta to feed the tube with the replacement valve first through the vein and then through the aorta to the heart. You may be able to stay awake during this procedure. This type of TAVR approach may benefit women, who often have smaller blood vessels than men.
Accessing the heart from the vessel under the clavicle, or collar bone, may be an option if you have had heart surgery before or if you have another condition that makes it difficult to access other parts of the chest.
Your doctor may use the carotid artery in the neck to feed the tube to the heart — called transcarotid access. This type of procedure is rare but may be used when other options will not work.
Another rare location is through the septum, the wall of tissue that separates the right and left atria of the heart. Your doctor reaches the damaged valve by guiding the tube through a blood vessel from your thigh to the heart. New approaches to TAVR are making the procedure available to more people.
Your doctor may ask you to stop taking certain medications

Patent Foramen Ovale Closures (PFO)
A PFO closure is a structural heart disease treatment to close a small hole called a foramen ovale between the upper two heart chambers (atria). Everyone is born with this hole, which keeps blood from circulating to the lungs before a baby is born.
In most cases, we are able to repair PFOs and ASDs using minimally invasive techniques that only require small incisions, eliminating the need to open the entire chest. In an operating room, the wall (septum) between the two upper chambers of the heart (atria) is closed with sutures or covered with a patch.

Cardioversion
Cardioversion is a treatment to restore a normal heartbeat when your heart is beating too fast or with an irregular rhythm. It's often used to treat atrial fibrillation, the most common kind of irregular beat.
During cardioversion, a machine is used to deliver low-energy shocks to the chest while the heart rhythm is monitored. Cardioversion is a medical procedure that uses quick, low-energy shocks to restore a regular heart rhythm.

Radio-Frequency Ablation
Radio-Frequency Ablation is a non-surgical technique, which eliminates parts of the heart’s abnormal electrical pathway, which is causing a rapid heart rhythm.
During this treatment, an electrode catheter is inserted into the heart. The catheter is positioned so that it lies close to the abnormal electrical pathway and then radio-frequency energy passes through the catheter. The tip of the catheter heats up in order to eliminate small areas of heart tissue that contain the abnormal electrical pathway. If successful, radio-frequency ablation may cure the problem of a rapid heart rhythm.

Electrophysiology Study
An Electrophysiology Study is typically performed in an EP lab or cath lab. These are specially equipped operating rooms that usually contain an X-ray machine capable of acquiring live X-ray video images (a fluoroscope), equipment to record electrical signals from the heart, a stimulator to electrically excite the heart and control the heart rate, and ablation equipment to destroy abnormal tissue. A 3D navigation system that tracks and records the catheter position and associated electrical signals may also be used.
The procedure may be performed awake under local anesthetic, or under general anesthetic. Monitoring equipment is attached including an automated blood pressure cuff and a pulse oximeter to measure the oxygen saturation of the blood. A peripheral venous cannula is generally inserted to allow medication to be given such as sedatives, anesthesia, or medication.
An access site that will allow catheters to be passed to the heart via an artery or vein is shaved and cleaned, usually in the groin. The blood vessels used to reach the heart (the femoral or subclavian veins, and sometimes the femoral artery) are punctured before a guidewire and plastic sheath are inserted into the vessel using the Seldinger technique.
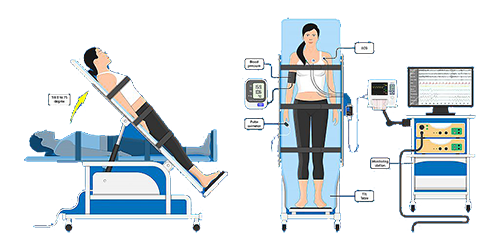
Tilt Table Test
A tilt table test is a diagnostic test used to help physicians determine the cause of unexplained fainting (syncope) or severe lightheadedness in a patient. There are a number of reasons a patient might faint, including low blood sugar (hypoglycemia), abnormal heart rhythms (e.g., tachycardia or bradycardia) or low blood pressure (hypotension).
The tilt table test assesses whether the patient is fainting as a result of a sudden drop in blood pressure. The change may be to a hyperactive reflex that causes the blood vessels to suddenly widen (dilate), which may be due to dehydration, emotional stress or standing upright for a prolonged period of time. This type of fainting is now known as neuro-cardiogenic syncope, although many physicians and patients still refer to it as vasovagal syncope.
The tilt table test is conducted on a pivoting table. By securing the patient on his or her back to the tilt table, and then tilting the table upright (head up and feet down), the factors leading to neuro-cardiogenic syncope may be simulated. This test is designed to detect orthostatic hypotension, one of the most common causes of fainting.
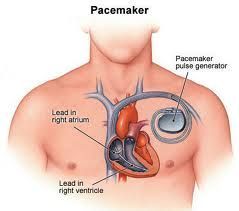
Pacemaker Insertion
A pacemaker is a lightweight, electronic device that monitors the heart’s electrical activity and delivers electrical pulses, as the heart needs them. If the pacemaker senses that the heart is beating too slowly or pauses for too long, the pacemaker stimulates the heart with precisely timed electrical pulses. The pacemaker is implanted into the body, usually beneath the skin in the upper chest just below the collarbone.

Implantable Cardioverter Defibrillator (ICD)
An Implantable Cardioverter Defibrillator (ICD) is an electrical device that continuously monitors our heartbeat and is implanted inside of the body, usually under the skin in the upper chest area just below the collarbone. When the device senses a dangerous rapid heart rhythm, it delivers one or more pulses or shocks to the heart and restores a more normal heart rhythm.
An ICD may be a treatment option following a carddiac arrest or a rapid heart rhythm problem that could lead to cardiac arrest. Placement of an ICD may allow a patient more freedom to participate in the activities of daily living.
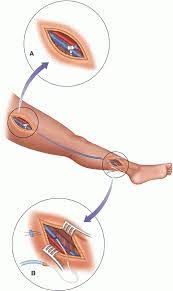
Venous Thrombectomy
A vascular surgeon or other vascular specialist performs thrombectomy in a hospital operating room. Just before the procedure begins, the patient is given an intravenous (through the vein) blood thinning agent called heparin.
The physician inserts a catheter sheath (short tube) through a small incision in the femoral vein in the groin or the popliteal vein below the knee. Contrast dye is injected through the sheath and venography is performed, allowing the physician to see the area of the vein being treated on an x ray screen.
The procedure takes approximately 2 to 3 hours.
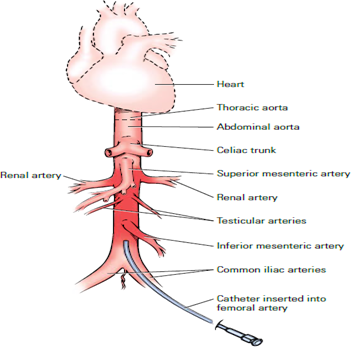
Aortogram
An Aortogram is an invasive diagnostic test using a catheter to inject dye (contrast medium) into the aorta. X-rays are taken of the dye as it travels within the aorta, allowing clear visualization of blood flow. This way, any structural abnormalities of the aorta will be accurately seen.
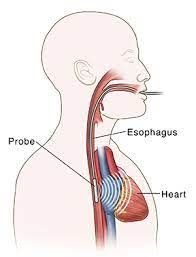
Transesophageal Echocardiogram (TEE)
An echocardiogram (often called "echo") is a graphic outline of the heart's movement, valves and chambers . During the transesophageal echocardiogram (TEE) test, an ultrasound transducer (which produces high frequency sound waves) provides pictures of the heart's valves and chambers and helps the physician evaluate the pumping action of the heart.
The ultrasound transducer is positioned on an endoscope (a long, thin, flexible instrument about 1/2 inch in diameter). The endoscope is placed into your mouth and passed into your esophagus (the "food pipe" leading from your mouth into your stomach) to provide a close look at your heart's valves and chambers without interference from the ribs or lungs.
TEE is often combined with Doppler ultrasound and color Doppler to evaluate blood flow across the heart’s valves. TEE is often used when the results from standard echo studies were not sufficient or when your doctor wants a closer look at your heart.
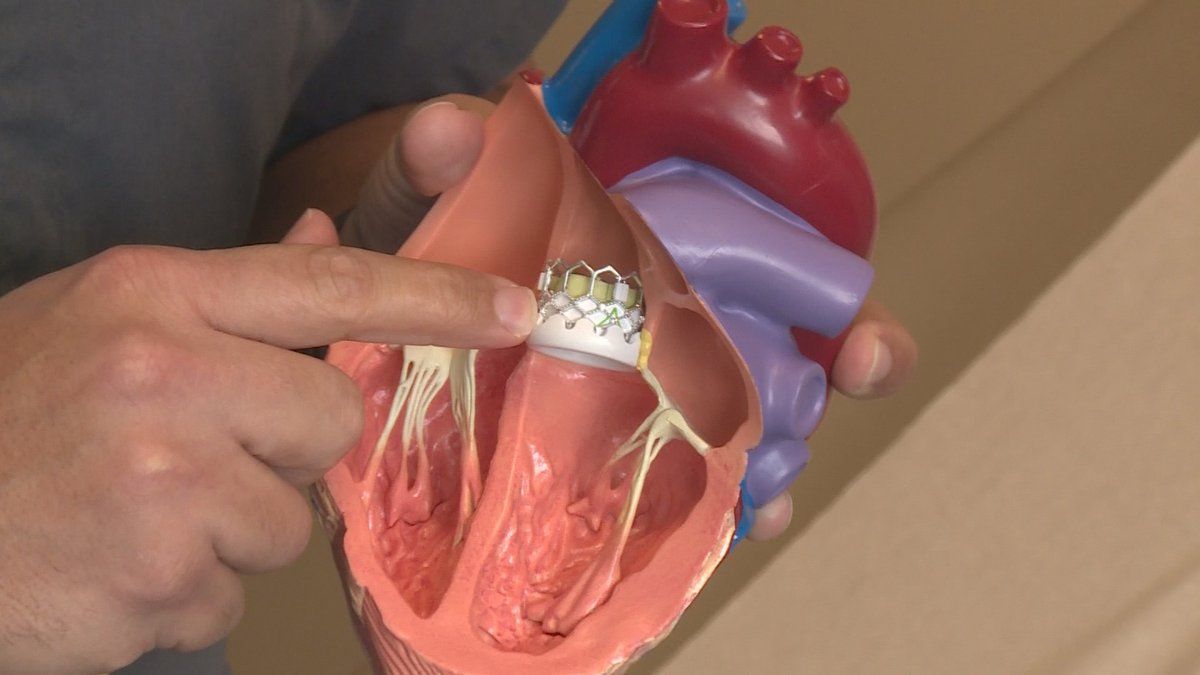
MitraClip
MitraClip is a procedure to fix your mitral valve.
During the procedure, doctors access the mitral valve with a thin tube (called a catheter) that is guided through a vein in your leg to reach your heart.
A small implanted clip is attached to your mitral valve to help it close more completely. This helps to restore normal blood flow through your heart.
Video Credit: Boulder Community Health
Watchman
A Watchman device is implanted into your heart in a one-time procedure. It’s a permanent device that does not have to be replaced and can not be seen outside the body.
To implant WATCHMAN, your doctor makes a small cut in your upper leg and inserts a narrow tube, as done in a standard stent procedure. Your doctor then guides WATCHMAN into the left atrial appendage (LAA) of your heart. The procedure is done under general anesthesia and takes about an hour. Patients commonly stay in the hospital overnight and leave the next day.
Video Credit: Boston Scientific
Our Mission
At San Diego Heart and Vascular Associates our mission is to improve the health of our community while providing excellent quality care to patients in a safe environment where people work together at their full potential to make a positive change.
SERVICES
Hospital Therapies
In Office Testing
QUICK LINKS
CONTACT
San Diego Office
619-297-0014
501 Washington St
Suite 512
San Diego, CA 92103
Coronado Office
619-435-1660
OFFICE HOURS
Monday - Friday: 8am - 5:30pm
Saturday - Sunday: Closed